Understanding Interim Life Safety Measures (ILSMs) in Healthcare
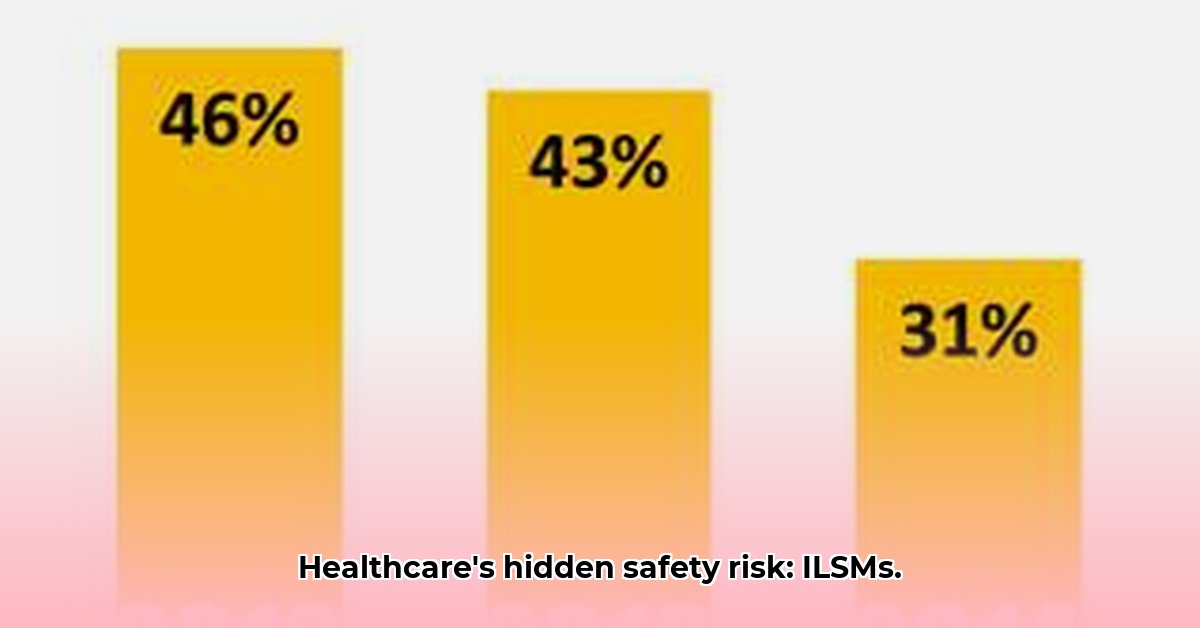
Maintaining patient, staff, and visitor safety is paramount in healthcare facilities. However, construction, renovations, or even routine maintenance can introduce temporary hazards. Interim Life Safety Measures (ILSMs) are temporary safety precautions implemented to mitigate these risks during periods of disruption. They act as a safety net, ensuring continued safe operations while permanent systems are unavailable or undergoing modifications. Understanding and implementing effective ILSMs is crucial for compliance and preventing accidents. What percentage of healthcare incidents are directly related to inadequate ILSMs? Studies suggest a significant portion, highlighting the critical need for proactive safety planning.
The Need for ILSMs: Protecting Against Construction, Renovation, and Non-Compliance Risks
Construction, renovations, and a failure to adhere to safety regulations can create significant hazards in healthcare settings. Unprotected exits, exposed wiring, and malfunctioning fire alarms represent just a few examples. Failing to implement adequate ILSMs during such periods can lead to severe accidents, potentially resulting in injuries, fatalities, and legal repercussions. A robust ILSM plan demonstrates a commitment to proactive safety and safeguards against these risks. According to Dr. Anya Sharma, Director of Safety at MetroHealth System, "A well-defined ILSM program isn't just about risk mitigation; it's about fostering a culture of safety that prioritizes the well-being of everyone in the facility.”
Developing a Comprehensive ILSM Policy: A Step-by-Step Guide
Creating an effective ILSM policy requires a structured approach. The following steps outline a process that aligns with Joint Commission standards and best practices:
1. Comprehensive Risk Assessment: Thoroughly assess all areas impacted by construction or renovation. Identify potential hazards (fire, falls, electrical, blocked exits, etc.) with specificity (e.g., "exposed wiring near patient rooms on the third floor"). Use checklists and risk matrices to document findings.
2. Precise Hazard Identification: Clearly define each identified hazard, noting its location, potential consequences, and affected populations. This detailed description helps in selecting appropriate mitigation strategies.
3. Effective Mitigation Strategies: Develop specific ILSMs to address each hazard. Examples include temporary fire barriers, clearly marked and accessible emergency exits, designated work zones with appropriate signage, and the use of Ground Fault Circuit Interrupters (GFCIs) (devices that detect ground faults and cut off power).
4. Robust Communication Plan: Establish a clear and efficient communication system to inform all stakeholders (staff, patients, visitors, contractors) about ILSMs. Utilize signage, training sessions, email announcements, and memos to ensure consistent and readily-available information.
5. Thorough Training Protocols: Conduct comprehensive training for all staff on ILSM procedures, including emergency responses and the proper use of safety equipment. Regular refresher training and drills are vital to maintain preparedness. How many facilities have documented training incidents resulting from inadequately trained staff? Data indicates that thorough training programs are a cornerstone of successful ILSM implementation.
Implementation and Monitoring: Ensuring ILSM Effectiveness
Implementing an ILSM plan is an ongoing process, not a one-time event. Effective implementation involves:
1. Regular Inspections: Conduct frequent inspections to verify the continued effectiveness of ILSMs. Use checklists to track compliance and identify any potential issues. Frequency of inspection should align with the individual hazard's risk level.
2. Detailed Documentation: Maintain comprehensive records of all ILSMs, inspections, training sessions, and incident reports. This documentation is crucial for demonstrating compliance and identifying areas for improvement.
3. Proactive Data Analysis: Regularly analyze inspection data and incident reports to identify trends and patterns. This data-driven approach helps refine the ILSM plan and address persistent issues. What percentage of facilities use data analysis to inform their ILSM improvement strategies? Best practice suggests nearly all high-performing facilities would utilize this strategy.
Addressing Challenges: Overcoming Obstacles in ILSM Implementation
Several challenges can hinder effective ILSM implementation. These include:
- Communication Barriers: Ensure clear, consistent, and multi-lingual communication to prevent confusion and misunderstandings.
- Limited Resources: Prioritize resource allocation towards high-risk areas and critical ILSMs.
- Staff Resistance: Address concerns and demonstrate the importance of ILSMs in protecting staff and patients. Open communication and leadership buy-in are crucial.
Continuous Improvement: A Dynamic Approach to Safety
The ILSM plan should be a living document. Regularly review and update it based on inspection findings, incident reports, changes in regulations, and best practices. This iterative process ensures the plan remains effective and adaptable to changing circumstances.
Conclusion: Prioritizing Safety Through Effective ILSMs
Effective ILSMs are essential for maintaining safety in healthcare facilities during periods of change. By following the guidelines outlined in this guide, healthcare facilities can create a safer environment for everyone, demonstrate compliance with regulatory requirements, and foster a culture of proactive safety.
Appendix (Optional): ILSM Policy Templates and Checklists
(This section would include downloadable templates for ILSM policies, risk assessment matrices, and inspection checklists.)